Breast cancer
Breast cancer: detect early, protect early
- Breast cancer is one of the most frequently diagnosed cancers in women worldwide.
- Changing reproductive patterns, physical inactivity and obesity are the prime fuelling factors.
- Breast cancer can be effectively managed if detected early.
- Increased awareness, routine examination, adopting a healthy lifestyle, completing the treatment regimen, rehabilitation and palliative care are key elements towards breast cancer care and control.
What happens to the breast tissue during breast cancer?
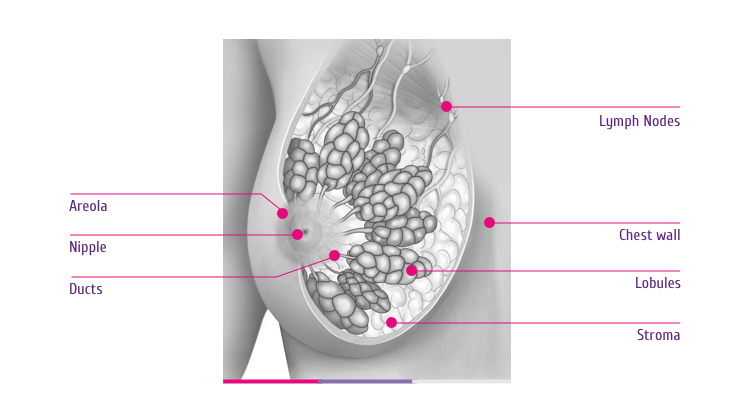
A normal female breast tissue is made up of glands and ducts mostly. These glands or ‘lobules’ can cause milk secretion, which is carried through the ducts to the nipple. Apart from these glands, there are fat, connective tissue, lymph nodes and blood vessels in the breast. Here is how a normal breast tissue looks like (Figure 1).
When the cells in these tissues start to divide uncontrollably and abnormally, it leads to a lump in the breast, which may lead to cancer. What exactly triggers such uncontrolled division in not yet clearly known. What is known are some potential risk factors. Know about these here.
Cancer can begin in the glands or the ducts. It can also begin in the lymph vessels in or around the skin of the breast, including armpits. At later stages, these cells can move out of its place of origin and invade the surrounding areas. This is when the cancer is called ‘invasive’ or, ‘infiltrating’.
Types
Are all breast cancers alike?
Breast cancer tissues from different patients do not always look alike. Depending upon the site of origin, stage or pattern of protein/gene expression, there exists differences. Accordingly, there are different sub-types to breast cancer.
Classifying breast cancer into different sub-types offers many advantages. One of these is that, it helps the doctors in selecting the most appropriate treatment and to make better predictions on the progress of the disease.
Here are some of the most commonly diagnosed sub-types:
Based on the site of origin or stage
I.Ductal carcinoma in situ (DCIS)
‘In situ’ means ‘in the original place’ in Latin. DCIS is a cancer where cells in the lining of the milk duct divide uncontrollably. It has not yet have become invasive. And so, is more treatable at this stage. However, having had DCIS at least once also increases the chances of its recurrence in the subsequent years.
II.Lobular carcinoma in situ (LCIS)
In LCIS, the cancer develops in the lobules (glands), which are at the end of the ducts. LCIS, which is not invasive yet, does not cause major symptoms.
III.Invasive (infiltrating) ductal carcinoma (IDC)
IDC is the most common sub-type of breast cancer, accounting for upto 80% of all the cases. Here, the abnormally dividing cells would have spread from the ducts to other parts of the breast, or body.
IV.Invasive (infiltrating) lobular carcinoma (ILC)
ILC begins in the milk-carrying ducts and spreads beyond it, to other parts of the breast, or body. ILC is the second most commonly reported breast cancer and tends to occur later in life than IDC.
V.Inflammatory breast cancer
Here, the cancer starts in the lymph vessels of the skin of breast. This leads to fluid build-up in the breast tissue, leading to inflammation. It is rare, but, aggressive; meaning that it progresses rapidly in the body, often within weeks or months. It is more likely to come back after treatment than other types of breast cancer.
Inflammatory breast cancer is reported more commonly in women who are obese, than in women with a normal BMI.
VI.Paget disease of the nipple
In this rare sub-type, cancer cells collect in and around the nipple area. It is often mistaken for some skin condition as symptoms include itching, tingling, redness, flaking, in the nipple area and abnormal nipple discharge.
Based on protein expression
Because of mutations, certain cancer cells overexpress specific receptor proteins inside or on their surface. This is another basis of classifying cancer cells. Many such patients can take the benefit of targeted therapy. To know more on targeted therapy, click here.
On this basis, breast cancer cells are classified into:
I.Luminal subtype
Cancer cells of this subtype appear like those in the inner lining of the mammary (breast) ducts. A majority of these cells overexpress estrogen receptors. Treatment of these tumors often employs hormone therapy (e.g. tamoxifen).
II.Basal subtype
The cells here look like those surrounding the outer (basal) cells of the mammary ducts. Most cells of this subtype are triple negative (TNBC; i.e., negative for the receptors of Estrogen, Progesterone and HER2) and are not suitable for any known targeted therapy.
III.HER2 subtype
A good majority of the patients of this subtype overexpress the HER2 receptor on the cell surface. HER2 positive breast cancers can be treated with HER2 targeting drugs (e.g., trastuzumab, pertuzumab, lapatinib, trastuzumab emtansine).
IV.Normal breast tissue-like
None of the above-mentioned molecular signatures could be identified in this subtype.
In addition, cancer can also be sub-divided depending on the stage of the disease. To read more on this, click here.
Abbreviations
- BMI : Body Mass Index
- DCIS : Ductal carcinoma in situ
- HER2 : Human epidermal growth factor 2
- HER2+ : Human epidermal growth factor 2 positive
- IDC : Invasive (infiltrating) ductal carcinoma
- ILC : Invasive (infiltrating) lobular carcinoma
- LCIS : Lobular carcinoma in situ
- TNBC : Triple Negative Breast Cancer
References
- Breast Cancer Journey, Third Edition, American Cancer Society, 2013
- Breast Cancer Clear & Simple All Your Questions Answered, Second Edition, American Cancer Society, 2016
- Rosen’s Breast Pathology, 4th Edition, S. A. Hoda, Edi Brogi, F. C. Koerner and P. P. Rosen, Lippincott Williams & Wilkins, 2014
- Diseases of the Breast, 5th Edition, J.R. Harris, M.E. Lippman, M. Morrow, C.K. Osborne, Lippincott Williams & Wilkins, 2014
- Breast cancer and abortion: collaborative reanalysis of data from 53 epidemiological studies, including 83 000 women with breast cancer from 16 countries, The Lancet , Volume 363 , Issue 9414 , 1007 – 1016, 2004
- American Cancer Society. Breast Cancer Facts & Figures 2017-2018. Atlanta: American Cancer Society, Inc. 2017
- Ganmaa D, Willett WC, Li TY, et al. Coffee, tea, caffeine and risk of breast cancer: a 22-year follow-up. Int J Cancer. 122(9):2071-6, 2008
- Jemal, A., Bray, F., Center, M. M., Ferlay, J., Ward, E. and Forman, D. (2011), Global cancer statistics. CA: A Cancer Journal for Clinicians, 61: 69–90. doi:10.3322/caac.20107
- Breastcancer.org. Types of Breast Cancer. Available from: http://www.breastcancer.org/symptoms/types
Risk factors
Who is at risk?
Here, you will read on what is known so far to put one at risk for breast cancer. But also know that, a set of risk factors may lead to cancer in one person, but not in the other – and we still do not know, why.
I.Age & Family history
Generally, there seems to be a risk with increasing age in women after 40. A family history (genetic pre-disposition) of breast cancer further increases the risk. Family history however, accounts for only a small portion of the total breast cancer burden.
II.Reproductive factors
Studies show that
- Early pregnancy confers a protective benefit.
- Increase in the number of childbirths, lowers the risk of incidence of breast cancer.
- Women with their first period before age 12 have higher breast cancer risk than those after age 14.
- Women who had their first full-term pregnancy after age 30 or who never had a full-term pregnancy are at increased risk of breast cancer.
- A late menopause increases the risk of breast cancer.
- Use of birth control pills (oral contraceptives) slightly increases the risk of breast cancer in and around the time of use of the pills.
- Breastfeeding lowers the risk of breast cancer.
III.Body weight
Gaining weight in adulthood (especially after menopause) increases the breast cancer risk.
IV.Lack of Exercise
Women who exercise regularly or are more physically active, have a lower risk of breast cancer than women who do not.
V.Other lifestyle factors
Eating food rich in carotenoids (the natural orange-red food pigment) such as apricots, carrot, pumpkin, spinach, tomato is reported to reduce breast cancer risk. Also, studies so far show that, with increase in the level of consumption of alcohol, breast cancer risk increases. About 4% of breast cancers in developed countries are attributable to alcohol. In addition, women working in night shifts for a long period of time have a moderately elevated risk of breast cancer.
Symptoms
What are the symptoms?
Here are some symptoms:
- One or more lumps or thickening in and around the breast (like the armpits)
- Feeling of heaviness, tenderness or burning of the breast
- Pulling in of the nipple
- Rash on the nipple that turns itchy, scaly or sore
- Nipple discharge that appears unusual
- A rapid onset of swelling, redness, darkening or inflammation in the breast (Redness covers at least a third of the skin)
- Peau d’orange skin: Peau d’orange is a French word that means ‘orange peel’. During inflammatory breast cancer, the breast skin may appear bruised with dimpled skin texture like that of an orange peel
- A rapid increase in breast size
But, remember, these changes need not always be indicative of cancer. For example, breast pain or nipple discharge could be the result of infections in the breast tissue. If you experience an unusual change, it is best to talk to your doctor.
Screening
What steps can one take to lower breast cancer risk?
The best way to lower breast cancer risk is to pro-actively manage the known risk factors itself. This includes promotion of healthy diet, regular exercise, control of alcohol intake and weight.
Adopting a preventive lifestyle does not totally eliminate the chances of breast cancer incidence. Here is where regular screening becomes important. Regular screening in turn aids early detection. Early detection is a crucial strategy to help improve the outcome of treatment methodology, with the best possible resources available. If you don’t know what breast cancer screening is, you can know this here.
Is it possible to detect breast cancer early? How?
It is possible to detect breast cancer early, if you perform routine screening and examination. The good news is that if detected & treated early, there are better chances of survival.
I.Mammography Screening
Mammogram is an X-ray photograph of the breast. All women should have access to mammogram screening especially when they, in consultation with their doctors, decide it is necessary based on the signs or symptoms or family history. Mammography helps in early diagnosis, making it easier to treat, also evaluate and follow progress of the disease and response to treatment.
According to the National Comprehensive Cancer Network (NCCN) guidelines, women above 25 years of age may be evaluated and broadly categorized into 2 groups – High risk category and Average risk category.
High risk category: The high risk category includes women with a prior history of breast cancer; or those with a family history of breast cancer; or with a known genetic pre-disposition to breast cancer; or those who have received radiotherapy in the chest area below 30 years of age. It is recommended that women in the high risk category get yearly mammography screening done after age 25.
Average risk category: Among the average risk category, for those between 25 to 39 years of age, mammography is recommended once in 3 years, while for women at and above the age of 40, an annual mammogram screening is recommended, according to the NCCN guidelines.
II.Clinical breast examination (CBE)
CBE refers to a careful examination of breasts by a trained and experienced health care professional. It is recommended that women below 40 years of age, have a CBE done every 3 years and those above 40 have it done yearly once.
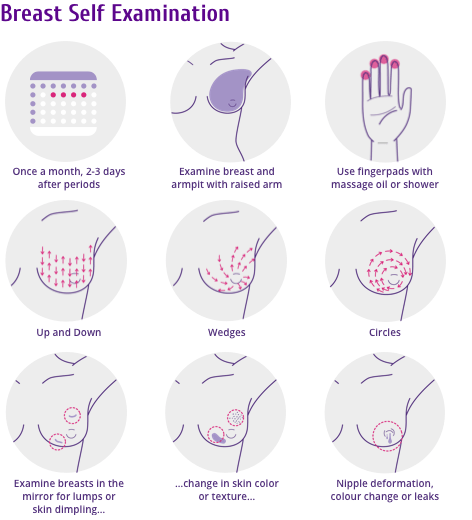
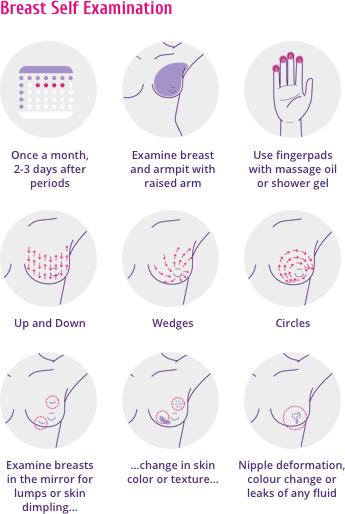
III.Breast self-examination (BSE)
The practice of regularly examining one’s own breasts is akin to taking responsibility of one’s own health. BSE can be regularly performed in addition to mammography screening or a CBE. One can do this at the end of regular monthly periods or for those after menopause, on the same date and time every month (Figure 1).
In BSE, one does a monthly self-check for any lumps or other abnormal changes in and around the breast (including armpits). BSE is not exactly a cancer screening tool, but at times, it can help locate a lump that might be otherwise too small, hence missed during routine tests. Given this, every lump thus found need not be cancerous.
IV.Magnetic Resonance Imaging (MRI)
MRI, that uses magnetic fields to take multiple images of the breast tissue for detailed analysis is helpful in screening for those who are at high risk for breast cancer.
Abbreviations
- BSE : Breast Self Examination
- CBE : Clinical Breast Examination
- MRI : Magnetic Resonance Imaging
References
- Berkey CS, Tamimi RM, Rosner B, Frazier AL, Colditz GA. Young Women with Family History of Breast Cancer and their Risk Factors for Benign Breast Disease. Cancer. 2012;118(11):2796-2803. doi:10.1002/cncr.26519.
- Rosner B, Colditz GA and Willett WC. Reproductive risk factors in a prospective study of breast cancer: the Nurses' Health Study. Am J Epidemiol. 139: 819-835, 199
- Transient Increase in the Risk of Breast Cancer after Giving Birth, Mats Lambe, Chung-cheng Hsieh, Dimitrios Trichopoulos, Anders Ekbom, Maria Pavia, and Hans-Olov Adami, N Engl J Med 1994; 331:5-9July 7, 1994DOI: 10.1056/NEJM199407073310102
- Moorman PG, Havrilesky LJ, Gierisch JM, et al. Oral contraceptives and risk of ovarian cancer and breast cancer among high-risk women: a systematic review and meta-analysis. J Clin Oncol. 31(33):4188-98, 2013
- Kushi, L. H., Doyle, C., McCullough, M., Rock, C. L., Demark-Wahnefried, W., Bandera, E. V., Gapstur, S., Patel, A. V., Andrews, K., Gansler, T. and The American Cancer Society 2010 Nutrition and Physical Activity Guidelines Advisory Committee (2012), American Cancer Society guidelines on nutrition and physical activity for cancer prevention. CA: A Cancer Journal for Clinicians, 62: 30–67. doi:10.3322/caac.20140
- Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat. 137(3):869-82, 2013
- A. Heather Eliassen, Sara J. Hendrickson, Louise A. Brinton, Julie E. Buring, Hannia Campos, Qi Dai, Joanne F. Dorgan, Adrian A. Franke, Yu-tang Gao, Marc T. Goodman, Göran Hallmans, Kathy J. Helzlsouer, Judy Hoffman-Bolton, Kerstin Hultén, Howard D. Sesso, Anne L. Sowell, Rulla M. Tamimi, Paolo Toniolo, Lynne R. Wilkens, Anna Winkvist, Anne Zeleniuch-Jacquotte, Wei Zheng, Susan E. Hankinson; Circulating Carotenoids and Risk of Breast Cancer: Pooled Analysis of Eight Prospective Studies. J Natl Cancer Inst 2012; 104 (24): 1905-1916. doi: 10.1093/jnci/djs461
- Hamajima N, Hirose K, Tajima K, et al. for the Collaborative Group on Hormonal Factors in Breast Cancer. Alcohol, tobacco and breast cancer—collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer. 87(11):1234-45, 2002
- Schernhammer ES, Kroenke CH, Laden F, Hankinson SE. Night work and risk of breast cancer. Epidemiology. 17(1):108-11, 2006.
- Breastcancer.org, The Five Steps of a Breast Self-Exam, Available from: http://www.breastcancer.org/symptoms/testing/types/self_exam/bse_steps
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines), Breast Cancer Screening and Diagnosis, Version 2.2018–May 18, 2018, NCCN.org
Diagnosis
If you suspect an abnormality in the shape and feel of your breast, consult your doctor immediately. An abnormality in the mammogram will also be a warning sign to get expert help.
Diagnosis is done with the help of follow-up tests. There can be a follow-up mammogram (diagnostic), breast ultrasound or a breast MRI. If there is a likelihood of cancer, your doctor may recommend a biopsy. During biopsy, a portion of the suspected tissue area is removed with a needle (needle biopsy) or a cut (surgical biopsy). This tissue is studied under the microscope by a pathologist.
Be patient while you wait for your test results. It is always good to get a second opinion for a more accurate diagnosis. And, remember, breast cancer survival rates are higher if detected early.
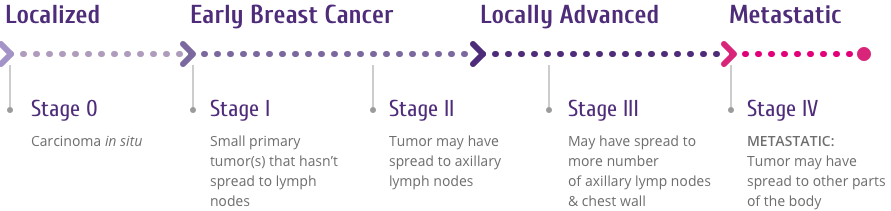
Staging of breast cancer
What are the different stages of breast cancer?
A combination of tests, as directed by your doctor, will help in staging of breast cancer.
Why is staging important? Knowing the stage of the cancer helps assess the extent to which it might have grown and spread. It also helps the doctor to determine the best treatment regimen.
Roughly, there are 5 stages to breast cancer, based on the pathology of three main determinants: the Tumor (T), the Node (N), and the extent of Metastasis (M). This method of staging breast cancer is called the TNM staging method (Figure 1).
Treatment
What are the available treatment options?
With promising research output worldwide, there is a considerable progress in the variety of treatment options available. This has in turn led to improved outcomes in breast cancer patients. It is a proven fact that, with a combination of effective breast cancer management measures it is possible to improve the survival rates too.
The treatment regimen that your physician chooses for you will depend on many factors. This includes: the tumor sub-type, stage of cancer, patient’s age, general health and presence of mutations, among others. Your doctor will decide and choose a combination of treatment modalities that will be well tolerated and achieve good treatment outcome. The treatment options available for you include:
I.Surgery
Whenever, surgery is required, depending on the spread of the cancer, your doctor may recommend a Lumpectomy (partial removal) or a Mastectomy (complete removal of breast). Surgery is often accompanied by radiation therapy. Thereafter, some women prefer going for a breast reconstruction surgery.
II.Radiation therapy
Surgery is often accompanied by radiation therapy (or, Radiotherapy) with an intent to kill any residual cancer cells and to prevent recurrence. During this, targeted, high-energy radiations (e.g. X-rays) are used to kill the cells in the area where cancer cells are present. However, radiation kills some of the adjacent normal cells also, resulting in side-effects. Some of this can be overcome with modern technologies though.
III.Systemic therapy
In contrast to localized treatment (as in the case of surgery and radiotherapy), systemic therapy refers to administration of the drug throughout the body (like for example, through the bloodstream). Systemic therapy can be recommended either before surgery (neoadjuvant therapy) or after surgery (adjuvant therapy). In case of large-sized tumors, neoadjuvant therapy may help shrink the tumor size. Whatever the case, the aim is to control the growth and spread of the cancer cells, which are otherwise not accessible by localized treatment.
Systemic therapy can be of different types: Chemotherapy, Hormone therapy or Targeted therapy. The choice is made based on factors that include size of the tumor, number of lymph nodes involved and the presence or absence of tumor-specific markers.
Chemotherapy
Chemotherapy is one of the most commonly advised treatment modalities. There is a whole array of chemotherapeutic drugs available today that kill cancer cells using varied mechanisms. They could be taken orally in a pill form or, can be injected into the vein (IV). Often, more than one such drug is used over a period of 3 to 6 months, with ample break time in between so as to allow the body to recover.
For example, in the case of HER2 positive breast cancers, the treatment regimen is often a combination of chemotherapy drug(s) and a HER2 targeting drug.
Example: Doxorubicin, Carboplatin, Cyclophosphamide, Paclitaxel, Docetaxel
Hormonal therapy
A proportion of breast cancers is hormone receptor positive. Most of the cells in this type of cancer have receptors for estrogen or progesterone. Hormonal therapy is often recommended in this case.
Hormonal therapy usually recommended is tamoxifen alone or in combination with aromatase inhibitor. (For e.g., Anastrozole, Exemestane)
Targeted therapy
In targeted therapy, the drug selectively target the cells by way of binding to a molecular marker or pathway specific to the cancer cells and later directs them to destruction. This thus results in little harm to the healthy cells.
Before administering targeted therapy, the cancer cells are tested for the presence of such markers. HER2 is a prominent marker in the case of HER2 positive cancers, which can be treated with HER2 targeting therapy. Some of the currently available HER2 targeting drugs are: trastuzumab, pertuzumab, lapatinib and trastuzumab emtansine. For this reason, it is crucial to check for the HER2 status in case of breast cancer. Know more here.
Abbreviations
- IV : Intravenous
- MRI : Magnetic Resonance Imaging
- TNM : Tumor Node Metastasis
References
- Brierley, J.D.; Gospodarowicz, M.K.; Wittekind, Ch., eds. (2017). TNM classification of malignant tumours (8th ed.). Chichester, West Sussex, UK: Wiley-Blackwell. ISBN 978-1-4443-3241-4.
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines), Breast Cancer, Version 3.2017–November 10, 2017, NCCN.org https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
- Radiation therapy and you: Support for people with Cancer, National Institutes of Health https://www.cancer.gov/publications/patient-education/radiationttherapy.pdf
- Targeted cancer therapy: the next generation of cancer treatment. Curr Drug Discov Technol. 2015; 12(1):3-20
HER2 positive breast cancer
What is HER2 positive (HER2+) breast cancer?
Breast cancer tissues from different patients, differ based on certain molecular markers they express. Two prominent markers expressed by breast cancers are Hormone receptors (HR) and HER2. Based on the expression of HR and HER2, breast cancer can be classified into 4 sub-types: HR+/HER2-, HR-/HER2+, HR+/HER2+, HR-/HER2-
The HER2 gene, that codes for HER2 protein is amplified in about 20% of breast cancer patients. This type of cancer is called – ‘HER2 positive breast cancer’. Cells in these types of cancers display more HER2 receptors on their surface, which cause them to grow aggressively and survive longer.
The mechanism by which HER2 overexpression leads to aggressive growth is complex. But, the knowledge of the overexpression in HER2+ breast cancers offers a promising bait strategy in treatment. Such an understanding is the basis of targeted therapy. In HER2 targeted therapy, biomolecules specially designed to have high affinity to the HER2 receptor are used. These molecules bind to HER2 overexpressing cells and direct them to destruction, with minimal damage to normal cells.
HER2 testing
What is HER2 testing? Why is it done?
If you have breast cancer, your doctor will recommend you to get HER2 testing done. This is to check for the presence, absence or the level of HER2 gene or protein in your biopsy sample. Your doctor might recommend HER2 testing at multiple times, before or during treatment, for several reasons.
How does this help? If your HER2 test result is positive, you can get the benefit of being treated with targeted drugs that specifically target and kill the HER2 positive cancer cells.
It is very important to have HER2 testing done and is in fact mandated by regulatory authorities such as the USFDA and the EMA.Here is how HER2 testing is done:
I. IHC testing (Immunohistochemistry)
Cells from a biopsy are stained and examined under a microscope to check for the presence and level of HER2 protein on the cell surface. IHC assigns a score of 0 to 3+ to the sample. A score of 3+ is HER2 positive.
II.FISH testing (Fluoroscence in situ hybridization)
In a FISH test, presence or absence, and the number of copies of the HER2 gene in the cells’ nucleus is measured. FISH test results will give a result of whether the cancer is ‘positive’ or a ‘negative’ (sometimes reported as ‘zero’) for HER2.
Treatment of HER2+ Breast cancer by targeted therapy
What are the treatment options available for HER2+ breast cancer?
Knowing that HER2+ cancer cells overexpress HER2 on their surface is akin to knowing the enemy. And, knowing the enemy is half the battle won. It thus helps in using the precise ammunition – in this case, a HER2 targeting drug.
HER2 targeting drugs are specially made to target the HER2 positive cells and mediate their destruction (directly or indirectly). They are very efficient and preferred as they act with little or no effect on the normal cells, thus, avoiding the side-effects of conventional chemotherapy.
Some known HER2 targeting drugs are: Trastuzumab, Pertuzumab, Trastuzumab emtansine and Lapatinib. Out of these, the first three are specially engineered monoclonal antibodies.
Although effective, these drugs might not work in some individuals. There can be serious side-effects. It is important that the patient is made aware of all possible side-effects. For this, feel free to talk to your doctor and take a second opinion if required.
Abbreviations
- EMA : European Medicines Agency
- FISH : Fluorescence in situ hybridization
- IHC : Immunohistochemistry
- USFDA. : United States Food and Drug Administration
References
- American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2016-2017. Atlanta: American Cancer Society; 2016
- Recommendations for Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Update Antonio C. Wolff, M. Elizabeth H. Hammond, David G. Hicks, Mitch Dowsett, Lisa M. McShane, Kimberly H. Allison, Donald C. Allred, John M.S. Bartlett, Michael Bilous, Patrick Fitzgibbons, Wedad Hanna, Robert B. Jenkins, Pamela B. Mangu, Soonmyung Paik, Edith A. Perez, Michael F. Press, Patricia A. Spears, Gail H. Vance, Giuseppe Viale, and Daniel F. Hayes, Journal of Clinical Oncology 2013 31:31, 3997-4013
What is Gastric cancer and Gastro-esophageal junction (GEJ) cancer?
Cancer that develops in the stomach is known as gastric cancer or stomach cancer, while cancer that develops at the junction of the stomach and the esophagus is termed gastro-esophageal junction (GEJ) cancer. Cancer of the gastro-esophageal junction is at present classified under esophageal cancers by the Union for International Cancer Control (UICC).
Adenocarcinomas are cancers developing in the inner lining of an organ. Over 90% or above of all gastric and GEJ cancers are adenocarcinomas. As of 2014, Gastric cancer is the fifth most commonly diagnosed cancer worldwide, while esophageal cancer stands at the eighth position.
Early cancerous changes in gastric and GEJ cancers begin in the inner lining of the stomach, which often progresses slowly. Due to this reason, it often goes undetected until advanced stages. At advanced stages, when the cancer starts spreading to other parts of the body, it is referred to as metastatic.
What are the known types of gastric cancer?
The 2010 WHO classification recognizes 4 types of gastric cancer patterns based on predominance and histology. These are:
- Tubular adenocarcinoma: These are the most common type among early gastric cancers and tend to form distended, fused or branching tubules of different sizes.
- Papillary adenocarcinoma: Reported in early gastric cancers, this type of cancer tends to affect older people and is often linked with liver metastasis. It is characterized by epithelial projections and a central fibrovascular core.
- Mucinous adenocarcinoma: This form accounts for 10% of gastric cancers. Histologically, more than 50% of the tumor contains extracellular mucinous pools.
- Singlet-ring cell carcinoma: More than 50% of this type of tumor shows isolated or small groups of cells containing intracytoplasmic mucin.
In addition, there are a few rare variants too. These include: adenosquamous carcinoma, squamous cell carcinoma and undifferentiated carcinoma.
What are the risk factors associated with gastric cancer?
Studies show that several factors influence the likelihood of occurrence of gastric cancer. These include:
- Helicobacter pylori infection (a bacteria found in the stomach, that can also cause stomach ulcers)
- History of benign polyp(s) in the stomach larger than 2 centimeters
- History of chronic atrophic gastritis
- History of pernicious anemia
- Obesity
- Consumption of alcohol
- Smoking
- High consumption of red meat
- High consumption of processed food
What are the symptoms of gastric cancer?
In most patients, the symptoms of gastric cancer may appear at an advanced stage. By this time, the cancer might have spread to other parts of the body. Commonly reported clinical symptoms include:
- pain in the upper central region of stomach
- bloating
- palpable mass in the upper central region of stomach
- nausea and vomiting due to obstruction of the gastric outlet
- early satiety (a state of feeling fed or gratified to capacity or beyond)
- dysphagia (difficulty in swallowing)
- upper gastrointestinal bleeding (due to ulceration of the tumor)
- Patients with metastasis may show clinical signs such as anorexia (abnormally low body weight), weight loss, jaundice, ascites (abnormal fluid accumulation in the abdomen) and hepatic enlargement
How is Gastric cancer diagnosed?
As mentioned earlier, gastric cancer often goes undetected until late stages. One of the main reasons for this could be patients who are on self-medication, and/or the symptoms being misunderstood as less serious gastrointestinal disorders.
However, early detection improves the outcome of treatment and quality of life. For example, with early detection, one could opt for endoscopic submucosal dissection or ESD. ESD is an effective and safe treatment mode, with benefits like lower late complication rate and shorter hospital stay.
Following tests help diagnose gastric cancer:
- Complete blood count to check for anemia
- Esophagogastroduodenoscopy (EGD) with biopsy
- Test for blood in stool
- Flexible spectral imaging color enhancement (FICE) endoscopy
- Chromo-endoscopy
- Computed Tomography (CT or CAT scan)
- Magnetic Resonance Imaging (MRI)
How is gastric cancer staged?
Staging helps determine the extent of spread of the cancer. This in turn helps in planning the best possible treatment strategy ahead on a case-to-case basis.
The staging system most often adopted and implemented is the one based on the TNM (tumor/node/metastasis) system, recommended by the American Joint Committee on Cancer (AJCC), based on the AJCC Cancer Staging Manual. Three key criteria are thus evaluated: the extent (size) of tumor (T), the spread of tumor to nearby lymph nodes (N) and the spread/metastasis to different sites of the body (M). Thereafter, gastric cancers are assigned different stages such as 0, 1A, 1B, II A, II B, III A, III B, III C, IV. Stage IV is the most advanced stage, where the cancer would have metastasized to different parts of the body.
What are the treatment options available for gastric cancer?
Treatment options advised for gastric cancer may include one or more of the following: surgery, chemotherapy, targeted therapy, and radiation therapy. In deciding a treatment mode in a given case, several factors are taken into consideration. This includes the stage of cancer, age and general state of health of the patient.
What is HER2 positive gastric cancer?
HER2 positive cancers display an elevated expression of HER2 receptors on their cell surface, when compared to normal cells. All the studies performed so far when put together, show that on an average, 17.9 % (i.e., slightly above one-fifth) of all gastric and GEJ cancers is HER2 positive.
A large number of studies also show that a HER2-positive status could be associated with decreased survival, tumor progression and metastases.
Further, elevated HER2 expression is utilized in targeted treatment of HER2 positive cancers to specifically target and destroy HER2 positive cells.
How is HER2 positive gastric cancer tested or diagnosed?
HER2 testing is an essential and integral part of decision making in devising a strategy for HER2 targeted treatment. If a biopsy sample is found cancerous, it is sent for HER2 testing.
During HER2 testing, the cancer sample is examined under the microscope, for the presence, absence and/or extent of HER2 protein and gene expression levels. This is assessed by the following methods:
- Immunohistochemistry (IHC)
- Fluorescence in situ hybridization (FISH)
Fluorescent in situ hybridization (FISH) is regarded as the gold standard for HER2 testing. However it comes with issues such as high cost and longer time taken in testing procedure. Hence, IHC screening is generally recommended first. Further, cases which seem doubtful or unambiguously positive are then recommended for a further FISH testing. Also, other simple alternatives to FISH are silver in situ hybridization (SISH), chromogenic in situ hybridization and dual-color dual-hapten in situ hybridization. The final testing strategy is devised by the physician case by case.
What is targeted therapy of HER2 positive gastric cancer?
After testing, if the cancer is found HER2 positive, targeted therapy is a recommended mode of treatment. In targeted therapy, the drug selectively targets HER2 positive cells for destruction, while causing less or minimal damage to normal cells.
Trastuzumab, an antibody which specifically targets and destroys HER2 positive cells, in combination with chemotherapy, is an approved first line therapy for HER2 positive metastatic gastric or gastroesophageal junction (GEJ) adenocarcinomas.
Abbreviations
- AJCC : American Joint Committee on Cancer
- EGD : Esophagogastroduodenoscopy
- FICE : Flexible spectral imaging color enhancement
- FISH : Fluorescence in situ hybridization
- GEJ : Gastro-esophageal cancer
- HER2 : Human epidermal growth factor 2
- HER2+ : Human epidermal growth factor 2 positive
- IHC : Immunohistochemistry
- SISH : silver in situ hybridization
- TNM : Tumor, Node, Metastasis
- UICC : Union of International Cancer Control
- WHO : World Health Organization
References
- Sobin, L. H., & Compton, C. C. (2010). TNM seventh edition: What's new, what's changed. Cancer, 116(22), 5336-5339. doi:10.1002/cncr.25537
- Dicken, B. J., Bigam, D. L., Cass, C., Mackey, J. R., Joy, A. A., & Hamilton, S. M. (2005). Gastric Adenocarcinoma: Review and Considerations for Future Directions. Annals of Surgery, 241(1), 27–39. http://doi.org/10.1097/01.sla.0000149300.28588.23
- Buas, M. F., & Vaughan, T. L. (2013). Epidemiology and Risk Factors for Gastroesophageal Junction Tumors: Understanding the Rising Incidence of This Disease. Seminars in Radiation Oncology, 23(1), 3-9. doi:10.1016/j.semradonc.2012.09.008
- Stewart, B. W., World Health Organization, International Agency for Research on Cancer, Organisation Mondiale de la Santé, World Health Organization, International Agency for Research on Cancer, & Centre International de Recherche sur le Cancer (Lyon). (2014). World cancer report. Lyon: IARC Press. ISBN (PDF) 978-92- 832-0443- 5; ISBN (EPUB) 978-92- 832-0432- 9
- Hamilton S.R., Aaltonen L.A. (Eds.): World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Digestive System. IARC Press: Lyon 2000
- Lin, S., Li, Y., Leung, K., Huang, C., & Wang, X. (2014). Salt Processed Food and Gastric Cancer in a Chinese Population. Asian Pacific Journal of Cancer Prevention, 15(13), 5293-5298. doi:10.7314/apjcp.2014.15.13.5293
- Zali, H., Rezaei-Tavirani, M., & Azodi, M. (2011). Gastric cancer: prevention, risk factors and treatment. Gastroenterology and Hepatology From Bed to Bench, 4(4), 175–185.
- NCCN Clinical Practice Guidelines in Oncology: Gastric Cancer (including the proximal 5 cm of the stomach). Version 2.2012, NCCN.org. Available at: http://www.isesnet.org/wp-content/uploads/2013/02/NCCN-gastric-2012.pdf
- Implementation of AJCC 8th Edition Cancer Staging System. American Joint Committee on Cancer. Available at https://cancerstaging.org/About/news/Pages/Implementation-of-AJCC-8th-Edition-Cancer-Staging-System.aspx.
- Abrahao-Machado, L. F., & Scapulatempo-Neto, C. (2016). HER2 testing in gastric cancer: An update. World Journal of Gastroenterology, 22(19), 4619. doi:10.3748/wjg.v22.i19.4619
- He, C. (2013). Correlation of human epidermal growth factor receptor 2 expression with clinicopathological characteristics and prognosis in gastric cancer. World Journal of Gastroenterology, 19(14), 2171. doi:10.3748/wjg.v19.i14.2171
- Jørgensen, J. T., & Hersom, M. (2012). HER2 as a Prognostic Marker in Gastric Cancer - A Systematic Analysis of Data from the Literature. Journal of Cancer, 3, 137-144. doi:10.7150/jca.4090
- Sugimoto, T., Okamoto, M., Mitsuno, Y., Kondo, S., Ogura, K., Ohmae, T., Koike, K. (2012). Endoscopic Submucosal Dissection is an Effective and Safe Therapy for Early Gastric Neoplasms. Journal of Clinical Gastroenterology, 46(2), 124-129. doi:10.1097/mcg.0b013e31822f3988
- Jeon, H. K., Kim, G. H., Lee, B. E., Park, D. Y., Song, G. A., Kim, D. H., & Jeon, T. Y. (2017). Long-term outcome of endoscopic submucosal dissection is comparable to that of surgery for early gastric cancer: a propensity-matched analysis. Gastric Cancer, 21(1), 133-143. doi:10.1007/s10120-017- 0719-4
- American Cancer Society® Tests for Stomach Cancer. Available from: https://www.cancer.org/cancer/stomach-cancer/detection-diagnosis-staging/how-diagnosed.html
- Li, Q., Jiang, H., Li, H., Xu, R., Shen, L., Yu, Y., … Liu, T. (2016). Efficacy of trastuzumab beyond progression in HER2 positive advanced gastric cancer: a multicenter prospective observational cohort study. Oncotarget, 7(31). doi:10.18632/oncotarget.10456
1.I suspect a thickening in my breast tissue. Could it necessarily be cancer?
No, not always. Finding a thickening (such as a lump or a cyst) in the breast does not necessarily mean that you have cancer. Consult a doctor for detailed medical examination and advice thereafter.
2.What are the symptoms of breast cancer?
Some commonly found symptoms of cancer are: lump, thickening or dimple in breast, nipple changes with or without abnormal discharge, pain in the breast, inversion of nipple, redness or scaling of breast skin etc. To know more, click here.
3.What is HER2 positive breast cancer?
The HER2 gene, that codes for HER2 protein is amplified in about 20% of breast cancer patients. This type of cancer is called – ‘HER2 positive breast cancer’. Cells in these types of cancers display more HER2 receptors on their surface, which cause them to grow aggressively and survive longer. This could be detected with specific tests in consultation with your doctor.
4.Is it true that breast cancer runs in families?
- Only few of the breast cancer cases are found to have passed on from an inherited gene. In other words, most of the women who have breast cancer have not inherited it from a family member. So, breast cancer does not ALWAYS run in families.
- But, if you have had a close family member with breast cancer, consider talking to your doctor to assess the possible risk factors.
5.What are the known causes of breast cancer?
- The real causes of breast cancer are not clearly known yet. It also varies from person-to-person.
- Having said that, changing reproductive patterns, physical inactivity and obesity have a heavy influence on the incidence. To know more, click here.
- Remember, breast cancer does not spread! Neither from a person, nor from a machine or air!
- If you are worried about your health, talk to your doctor to discuss and work on the risk factors, if any.
6.What is the best I can do to protect myself from breast cancer?
- Be aware of the risk factors that could lead to breast cancer and adapt a healthy lifestyle as a preventive action.
- Exercise regularly, or be physically active. Eat healthy, with plenty of fruits, green & orange-red vegetables and food rich in carotenoids (like apricots, melons, carrots, beetroot, sweet potatoes, spinach) in your diet. Alcohol, if consumed, must be in moderation.
- Together with these, it is recommended that you undergo a regular check-up for breast cancer. To know more on this, click here.
- Detect early, protect early!
7.What effect does my menstrual or reproductive history have on breast cancer risk?
- Women who have had their first menstrual cycle before age 12, or have no biological children, or gave birth to their first child above age 30, or had menopause above age 55 have been shown to be at a higher risk of breast cancer.
- In other words, research has shown that the more the number of menstrual cycles a woman has had, the higher is the risk.
8.How often should one do a breast self-examination (BSE)?
It is recommended that one does a BSE once every month. The best time to do this is soon after the menstrual period. For those no longer menstruating, it should be done once monthly, preferably on the same date each month. However, it is not enough to rely on BSE alone, as BSE by itself is not exactly a breast cancer screening tool. It should be accompanied with Clinical Breast Examinations (CBE) and mammography screening by trained personnel.
9.Is mammography painful?
During mammography, the breast is compressed between two plates, so as to capture an X-ray image. This might cause some discomfort. One can schedule the mammography a week after the menstrual cycle, during which, the breast tissue is less sensitive. If you are concerned, talk to your doctor on any medicine you could take to feel less discomfort. Most importantly, take deep, slow breath during the procedure to feel relaxed.
10.Does wearing a bra increase breast cancer risk?
No studies so far associate this to breast cancer.
11.What are the side-effects of chemotherapy?
The side-effects of chemotherapy varies from person to person. It depends on how well a particular drug is tolerated by the body. Some common side-effects are nausea, vomiting, hair-loss, anemia, fatigue, infertility, taste and smell changes, irritated bladder, swelling and soreness all over the body, numbness and aching of the joints, hands and feet etc. Talk to you doctor to help manage the side-effects.
12.I have been diagnosed with breast cancer. Are there any foods that I should avoid?
Consult your doctor for advice that best suits your health condition. All the same, some healthy diet and lifestyle changes can still be proactively adopted:
- It is important that you strive to maintain a weight appropriate for your age and height
- Although there is no dietary pattern that can improve breast cancer survival, foods rich in carotenoids are highly recommended. (like melons, apricot, carrots, beetroot)
- Eat a good portion of fruits and vegetables every day
- Limit red meat or processed meat
- Limit consumption of ‘unhealthy’ fat (like fatty cuts of beef, pork, lamb; poultry skin; high fat dairy foods like whole milk, butter, ice cream)
- Try and consume more of ‘good’ fats (like whole eggs, nuts, fatty fish, avocado, dark chocolate, olive oil
- Limit consumption of alcohol
- Go for whole grain foods
13.Lately, I am experiencing frequent stomach pain with an unexplained weight loss. Could it be stomach cancer?
- Frequent stomach pain with an unexplained weight loss, despite not having changed your eating or exercise habits, can be a cause of concern. However, it need not necessarily be stomach cancer. It could also be due to a variety of conditions including celiac disease, diabetes, stress etc. Consult your doctor immediately to rule out the possibilities.
- Often, symptoms of gastric cancer go undetected until advanced stages of the disease. Hence, it is important to consult the doctor as soon as you notice a symptom. To know more on other symptoms of gastric cancer, click here.
14.I have a history of stomach polyps. Am I at risk of having stomach cancer?
- Stomach polyps are masses of cells that form in the inner lining of stomach. Most stomach polyps do not become cancerous. However, a history of such benign polyp(s) in the stomach larger than 2 centimeters can increase the risk of stomach cancer in future. To know of the other predominant risk factors, click here.
References
- Berkey CS, Tamimi RM, Rosner B, Frazier AL, Colditz GA. Young Women with Family History of Breast Cancer and their Risk Factors for Benign Breast Disease. Cancer. 2012;118(11):2796-2803. doi:10.1002/cncr.26519.
- Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat. 137(3):869-82, 2013
- A. Heather Eliassen, Sara J. Hendrickson, Louise A. Brinton, Julie E. Buring, Hannia Campos, Qi Dai, Joanne F. Dorgan, Adrian A. Franke, Yu-tang Gao, Marc T. Goodman, Göran Hallmans, Kathy J. Helzlsouer, Judy Hoffman-Bolton, Kerstin Hultén, Howard D. Sesso, Anne L. Sowell, Rulla M. Tamimi, Paolo Toniolo, Lynne R. Wilkens, Anna Winkvist, Anne Zeleniuch-Jacquotte, Wei Zheng, Susan E. Hankinson; Circulating Carotenoids and Risk of Breast Cancer: Pooled Analysis of Eight Prospective Studies. J Natl Cancer Inst 2012; 104 (24): 1905-1916. doi: 10.1093/jnci/djs461
- Hamajima N, Hirose K, Tajima K, et al. for the Collaborative Group on Hormonal Factors in Breast Cancer. Alcohol, tobacco and breast cancer—collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer. 87(11):1234-45, 2002
- Rosner B, Colditz GA and Willett WC. Reproductive risk factors in a prospective study of breast cancer: the Nurses' Health Study. Am J Epidemiol. 139: 819-835, 1994
- Chen L, Malone KE, Li CI. Bra wearing not associated with breast cancer risk: a population-based case-control study. Cancer Epidemiol Biomarkers Prev. 23(10):2181-5, 2014.
- Breast Cancer Clear & Simple All Your Questions Answered, Second Edition, American Cancer Society, 2016
- Zali, H., Rezaei-Tavirani, M., & Azodi, M. (2011). Gastric cancer: prevention, risk factors and treatment. Gastroenterology and Hepatology From Bed to Bench, 4(4), 175–185.